lun, 5 fév 2024
GLP-1 Drugs: A Costly Revolution in Obesity Treatment.
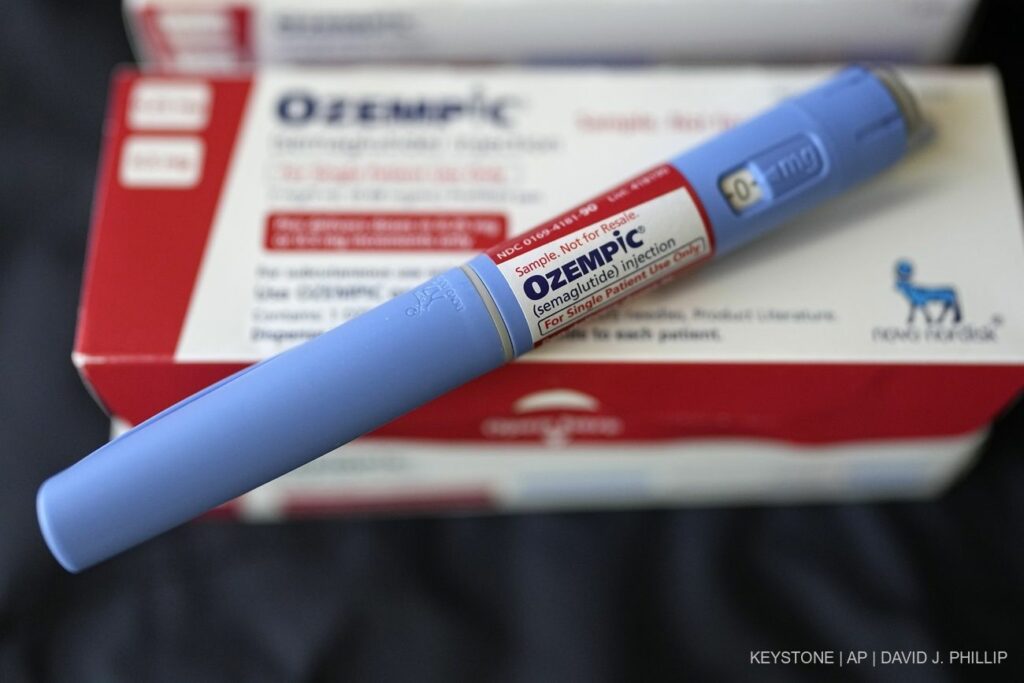
Drugs with a punch like the new GLP-1 drugs inevitably lead to discussions about their cost. As only Eli Lilly and Novo Nordisk have approved drugs on the market so far, they have a certain amount of pricing power.
The cost of Wegovy (semaglutide) from Novo Nordisk is 1349 US dollars per pack and month, while the cost of Mounjaro (tirzepatide) from Eli Lilly is just under 1100 US dollars.
In the short term, the drugs will undoubtedly drive up costs. According to the data currently available from Helsana for Switzerland, the costs for the active ingredient semaglutide for the treatment of diabetes and obesity amounted to just under CHF 52 million in 2021 and CHF 81 million in 2022.
“These medications are already driving up the costs of basic insurance and will certainly continue to do so,” predicts Manuel Elmiger, health economist at Helsana, in an interview with AWP. However, it is difficult to make assumptions about the extent of this. You have to look at how many people are obese and how market availability develops.
“If the majority of patients could reduce their weight significantly and in the long term, this would save costs for the treatment of secondary diseases,” the expert continued. Long-term use has not yet been investigated.
A similar sentiment is echoed by Lombard Odier: “Given the number of patients affected by obesity and the price of GLP-1 drugs (around USD 15,000 per patient per year in the United States), these treatments represent a new challenge for healthcare systems and payers. Drug manufacturers are now conducting clinical trials to demonstrate the positive effects of GLP-1 drugs beyond simple weight loss and cosmetic effects and to convince healthcare systems to reimburse the costs.
A recent study with Novo’s Wegovy showed that the number of cardiovascular events (heart attacks or myocardial infarctions) fell by 20 percent; another study showed that the drug slowed the progression of chronic kidney disease and reduced the risk of death from kidney failure. Further clinical studies are underway. “So it’s about getting payers to consider the total cost of healthcare expenditure per patient, with the prospect of reducing healthcare costs for obesity-related diseases, even though the cost of treatment may increase.”
Marco Bueter, Head of Surgery at the Zurich Obesity Center (USZ), is somewhat more critical. Although he sees the new methods as a welcome addition to the existing treatment options, he also warns of the costs. For example, although a surgical procedure represents a one-off higher expense for the payer, the follow-up costs are clearly lower than with the new drugs. In case of doubt, these would have to be taken for life.
©Keystone/SDA
